When it comes to COVID-19, the disease caused by the novel coronavirus (SARS-CoV-2), people over the age of 60 years old and adults of any age with one or more chronic medical conditions are considered to be “at risk.” This means they are more likely than other groups to develop a severe COVID-19 illness, according to the World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC). This is especially true for people who have a chronic respiratory illness, such as asthma.
If you have asthma, here is what you should know about COVID-19 and how you can protect yourself.
What we know about asthma and COVID-19
Asthma is a pre-existing lung condition affecting 1 in 13 people in the U.S. It can cause wheezing, chest tightness, coughing, and shortness of breath. Asthma can be controlled by taking medications and avoiding triggers.
COVID-19 is a respiratory disease caused by the SARS-CoV-2 virus. The virus affects cells in the airways, from the nose and throat down to the deepest parts of the lungs. In the nose and throat it might cause symptoms of a cold. In the upper airways, it might cause some breathlessness and cough. When the coronavirus lodges itself deep in the lungs, this is when things can start to get serious. Here, the coronavirus commonly causes a double lung infection, or bilateral pneumonia.
Interestingly, research so far does not suggest any link between having asthma and getting a more severe COVID-19 illness, or between asthma and coronavirus deaths.
Whether this is because the SARS-CoV-2 virus doesn’t affect people with asthma in the same way as other respiratory viruses, or because there simply isn’t enough data yet, remains to be seen.
Are people with asthma at higher risk of getting COVID-19?
So, there is no hard evidence that people with asthma get sicker with COVID-19 (yet). But is there any evidence that people with asthma are more likely to catch the coronavirus? Again, not that we are aware of. A study of 140 cases showed no link between coronavirus infections and asthma.
Some people with asthma may wonder if they are “immunocompromised” and what that means. Immunocompromised means that your immune system is weakened, either by a disease or by a medication. It means you are more likely to catch an infection and more likely to have a more severe illness than someone who is not immunocompromised.
Some people with asthma can be immunocompromised because of the medication they take. Here are some asthma medications and treatment combinations that can blunt the immune system:
- Any biologic therapy such as omalizumab (Xolair)
- Daily corticosteroid tablets or liquid
- Antibiotic tablets or liquid taken for asthma every week (e.g., azithromycin)
- Tiotropium (Spiriva), a prescription asthma medication
- A combination inhaler that contains a high daily steroid dose
- Taking an inhaler with a high daily steroid dose and montelukast (Singulair) together
Check with your provider if you’re not sure about whether your medications could be making you immunocompromised.
Are people with asthma at higher risk of poor outcomes from COVID-19?

Despite the lack of hard data, the WHO, the CDC, and lung disease specialists are in agreement: People with asthma have a higher risk of severe illness and death with respiratory infections in general. Because of this, any child or adult with moderate to severe asthma should consider themselves “at risk” for severe COVID-19 disease and take extra precautions with their health.
This is especially true for anyone who has been admitted to the hospital for asthma in the last 12 months, or who has ever been admitted to an intensive care unit for their asthma.
Why is this recommendation in place when there is no hard evidence? Here’s why.
Any infection in the lung can trigger an asthma attack, causing the smallest airways in the lung to tighten up and let very little air in and out. The symptoms are sudden and severe: shortness of breath, wheezing, and cough. If the infection is mild, for example with a common cold, asthma symptoms can usually be managed at home. Most people with asthma have an asthma action plan that tells them how to manage their symptoms when they get worse, and when to seek medical attention.
If the infection is more serious, a person with an asthma attack may need emergency treatment in the hospital with oxygen, nebulizers, and corticosteroids. Usually things improve pretty quickly. Antibiotics help to treat a bacterial lung infection if there is one, and flu treatments like Tamiflu can help shorten symptoms if the infection is caused by the flu.
With coronavirus (COVID-19), there are no antibiotics or antivirals that can cure the disease — yet. And so, if a person with asthma gets infected and develops a lung infection, health professionals worry that they are more likely to have a severe illness than healthy people. This is a risk that the medical community prefers not to take.
Should I be extra cautious about coronavirus if I have asthma?
Yes. The CDC has released new guidelines for people with asthma, which include the following:
- Stock up on supplies in case you need to self-isolate (a 14- to 30-day supply).
- Stay at home and practice social distancing from those you do not live with (about 6 feet).
- Avoid people who are sick, and wash your hands often.
- Avoid crowds.
- Avoid non-essential travel.
- Clean and disinfect your home and car regularly, especially items you touch often like doorknobs, light switches, cell phones, keyboards, faucets, car door handles, and steering wheels.
- If someone in your home is sick, stay away from them.
- Avoid sharing personal household items such as cups and towels.
The best way to protect yourself is to keep on top of your asthma and asthma symptoms. Follow these simple asthma management steps:
- Keep taking your inhalers exactly as prescribed to prevent an asthma attack if you do get infected by the coronavirus.
- Keep your fast-acting bronchodilator (such as albuterol) with you every day, in case your asthma symptoms get worse.
- Plan for an emergency supply of medications with your provider.
- Make sure you have an asthma action plan to help you recognize and manage asthma symptoms if and when they come on.
- Get a peak flow meter (from a pharmacy) and keep a diary of your peak flows and your symptoms. This can help track your symptoms and tell the difference between your asthma symptoms and new COVID-19 symptoms. It can also help your medical team to assess you over the phone or video.
- Anxiety and stress can make asthma symptoms worse. This is a time of high anxiety and concern for us all. Take steps to help manage your emotions.
General precautions for people with respiratory conditions
General tips for those with chronic respiratory illnesses such as asthma, chronic obstructive pulmonary disease (COPD), idiopathic pulmonary fibrosis, and cystic fibrosis include the following:
- Take your medication as prescribed and manage your symptoms as well as you can.
- Get the flu shot. If you have flu symptoms (cough, fever, muscle aches, congestion) call your doctor. There are treatments for the flu. However, a flu shot will not protect you against COVID-19.
- Get the pneumococcal vaccine (for bacterial pneumonia) if recommended by your provider. This will also not protect you against COVID-19, though.
- If you smoke, there’s never been a better time to stop. Smoking will increase your risk of severe illness and death from COVID-19.
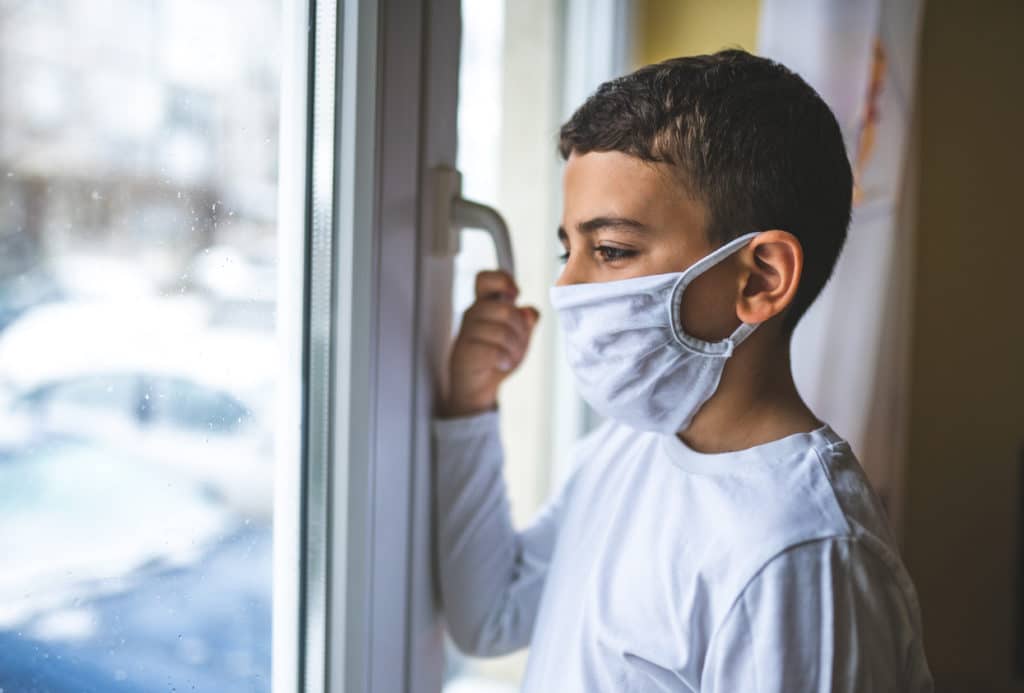
Should people with asthma wear a disposable mask when in public areas?
The CDC now recommends that everyone wear cloth face coverings in public settings where social distancing can be difficult (for example, in grocery stores and pharmacies.) This is true whether you have asthma or not. People should also wear a face mask at home if they are looking after someone who has or could have COVID-19.
This article originally appeared on GoodRx.com

Dr. Sophie Vergnaud, MBBS
Clinical Physician
Clinical expert on the GoodRx Research team. She specializes in pulmonology and all things internal medicine.


